Standard of care PsA
Striving for and achieving high treatment targets is linked to substantial benefits for your SpA patients in terms of:
Quality of life
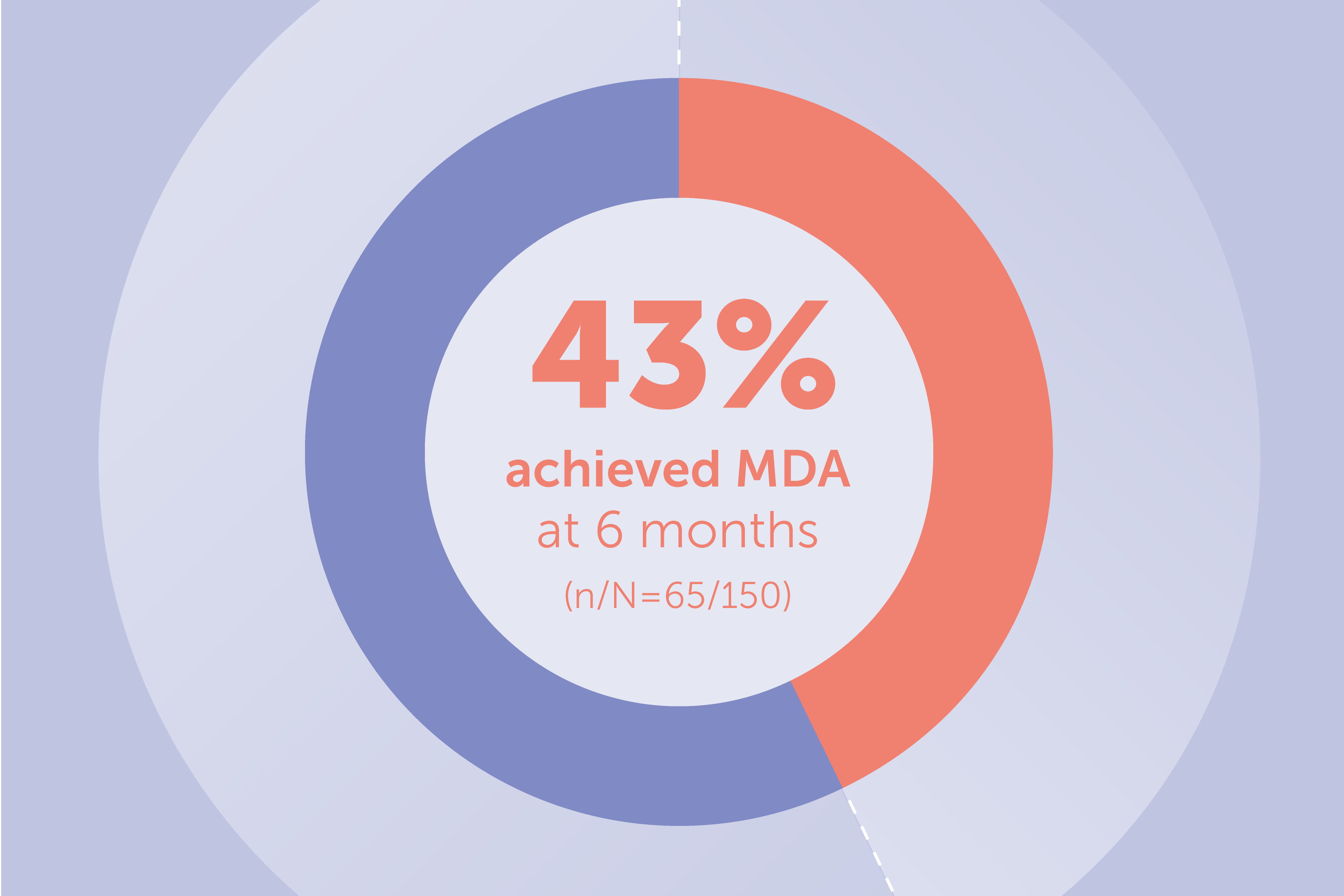
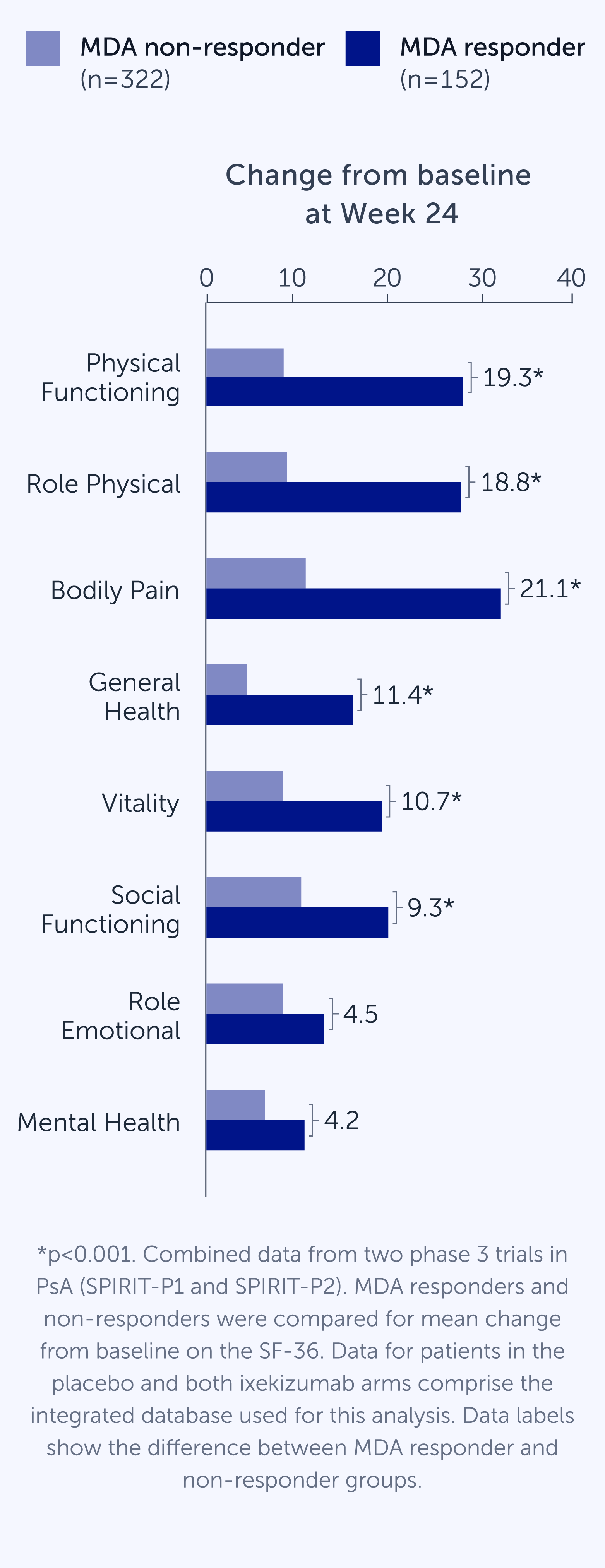
Achieving MDA in PsA is associated with significant improvements in 6 of the 8 SF-36 domains, including physical functioning, pain and general health1
Structural progression
Patients who achieve sustained MDA show significant reductions in radiographic progression compared to patients who never achieve MDA²
Patient function
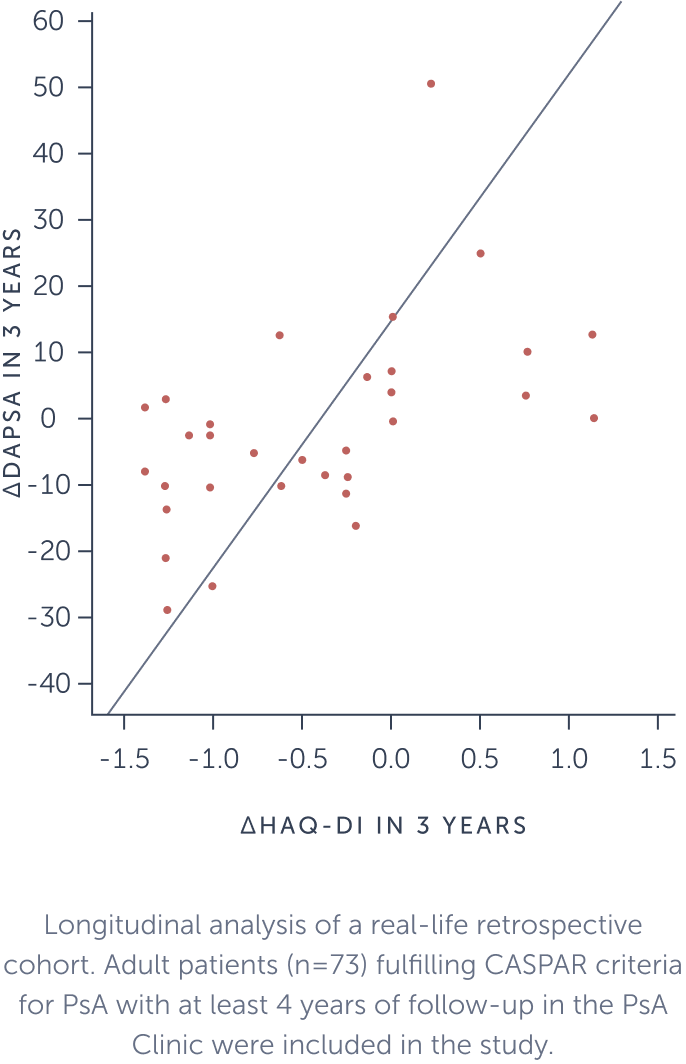
Changes in DAPSA are significantly correlated with a change in the HAQ-DI and patients in DAPSA remission show a constant decline in HAQ-DI scores, thus improved functionality, during 6 years of follow-up³
Achieving MDA improves patient quality of life¹
Achieving MDA in PsA is associated with significant improvements in 6 of the 8 SF-36 domains, including physical functioning, pain and general health.
Achieving sustained MDA reduces the risk of structural progression in PsA patients²
Patients who achieve sustained MDA show significant reductions in radiographic progression compared to patients who never achieve MDA.

Greater disease control is associated with improved functionality³
Changes in DAPSA are significantly correlated with a change in the HAQ-DI and patients in DAPSA remission show a constant decline in HAQ-DI scores, thus improved functionality, during 6 years of follow-up.
Speak with a member of our medical team.
If you have questions or want to know more, please reach out to our medical team.
- 1
- Adapted from Coates LC et al. BMC Rheumatol. 2018;2:24.
- 2
- Adapted from Kavanaugh A et al. Arthritis Care Res. 2016;68(2):267–274.
- 3
- Adapted from Cruz LV et al. EULAR 2020. Abstract AB0843.
- CASPAR
- classification criteria for psoriatic arthritis
- DAPSA
- disease activity index for psoriatic arthritis
- HAQ-DI
- health assessment questionnaire-disability index
- MDA
- minimal disease activity
- PsA
- psoriatic arthritis
- SF-36
- 36-Item Short Form Survey
- SHS
- Sharp/van der Heijde Score
- SpA
- spondyloarthritis